When people first hear about retinal problems, two questions often come up.
How common are retinal tears?
How common is retinal detachment?
Both conditions are serious, but they are not equally common.
Retinal tears are more frequent than full retinal detachments.
Certain groups of people have a higher risk than others.
This article explains how often retinal tears and detachments occur, who is more likely to develop them, and why knowing your risk matters.
This article is for general information only and is not medical advice.
Any new flashes, floaters or a curtain over your vision need same-day eye care.
Explore: The Best Healthcare SEO Agencies for Doctors in 2026
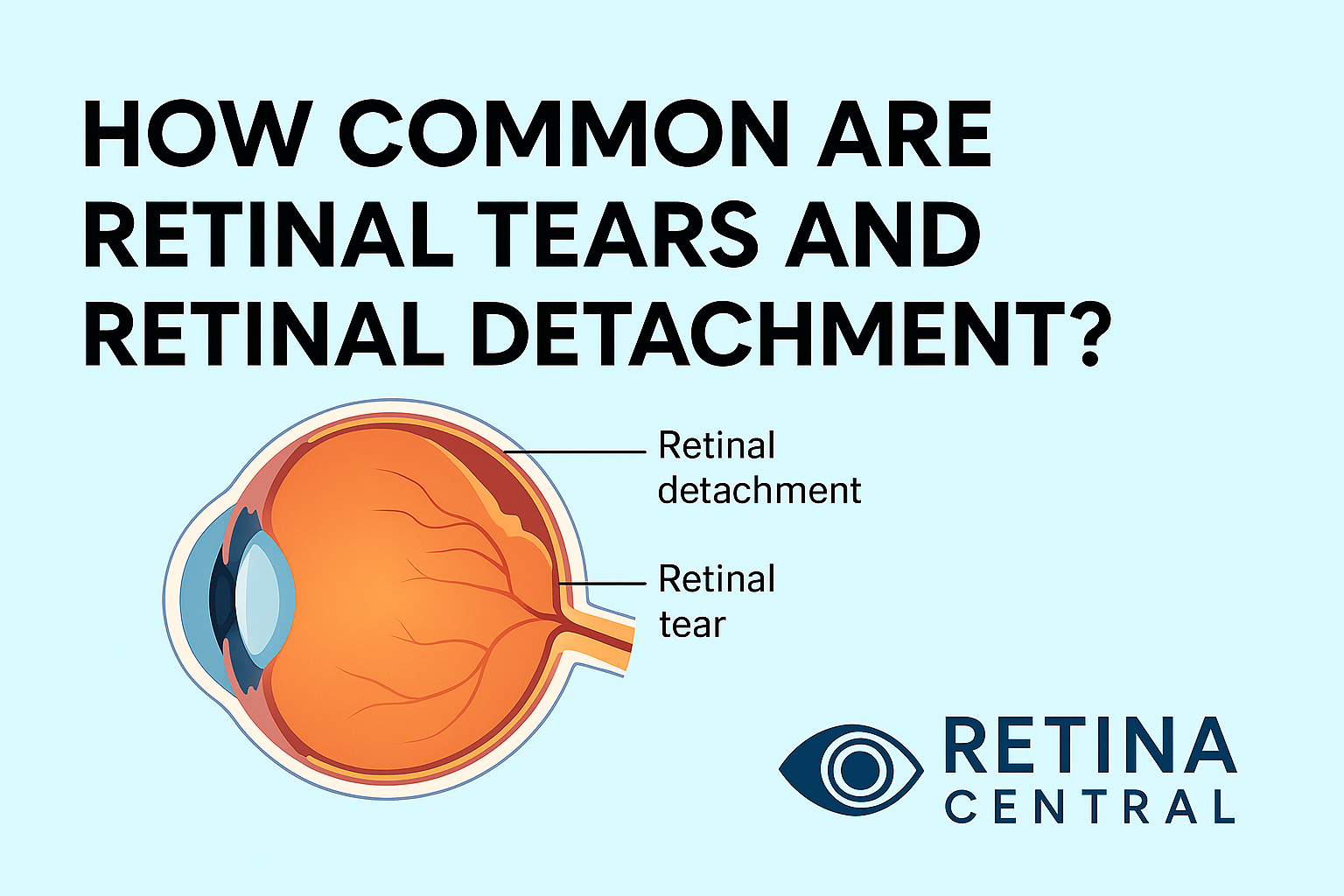
What Is a Retinal Tear?
The retina is a thin, light-sensing layer that lines the back of the eye.
It captures light and converts it into signals that travel along the optic nerve to the brain.
Inside the eye is a clear gel called the vitreous.
With age, this gel can shrink and pull away from the retina in a process called a posterior vitreous detachment.
Most of the time, this process is harmless.
If the vitreous tugs too strongly on the retina, it can cause a small rip or hole.
This rip or hole is called a retinal tear.
A tear is an early problem that can lead to a more serious one, retinal detachment, if fluid passes through the tear and lifts the retina away from the wall of the eye.
How Common Are Retinal Tears?
Retinal tears are not rare, especially in people with certain risk factors.
Retinal tears are more common in people with high myopia, also called strong near-sightedness.
Longer eyes with stretched retina are more vulnerable to tearing.
Retinal tears are more common in older adults.
As the vitreous gel changes with age, it is more likely to pull on the retina.
Retinal tears are more common in people who have already had a tear or detachment in the other eye.
If one eye has had a problem, the other eye may have similar structural risk.
Retinal tears are more common in people with areas of thinning in the peripheral retina, such as lattice degeneration.
These thin areas can tear more easily when the gel shifts.
Retinal tears can also appear after eye trauma or surgery.
A strong blow to the head or eye can damage the retina directly.
Many small tears may never cause symptoms and may only be seen during a detailed eye examination.
Others cause flashes, floaters or vision changes that lead people to seek help.
In summary, retinal tears are relatively common in higher risk groups, and less common in the general population.
The key point is that a tear is important not because of how often it happens, but because of what it can lead to if it is not treated.
How Common Is Retinal Detachment?
Retinal detachment is less common than retinal tears, but more dangerous for sight.
Not every retinal tear turns into a detachment.
The risk that a tear will progress depends on its size, its location, the amount of traction from the vitreous gel and whether there is bleeding or fluid getting behind the retina.
Retinal detachment is more likely in people with the same risk factors seen in retinal tears.
Retinal detachment is more likely in people with high myopia.
Retinal detachment is more likely after trauma or serious eye injury.
Retinal detachment is more likely after certain types of eye surgery.
Retinal detachment is more likely in people with a family history of detachment.
Even among these higher risk groups, most people will not experience a detachment in their lifetime.
However, for the people who do, the impact can be life changing.
That is why awareness of symptoms and quick action matter more than exact percentages for any individual.
How Often Do Retinal Tears Turn into Retinal Detachments?
Not every retinal tear leads to a detachment.
Some tears remain stable for years, while others progress quickly.
Several factors influence the chance that a retinal tear will cause detachment.
Large or horseshoe-shaped tears are more dangerous than small round holes.
Tears with bleeding into the vitreous cavity suggest stronger traction and higher risk.
Multiple tears or widespread lattice degeneration increase the overall risk.
Because it is impossible to predict exactly which tear will progress, eye doctors take retinal tears seriously.
They often recommend laser or freezing treatment to create a firm scar around the tear.
This scar helps seal the retina down and lowers the chance of detachment.
From a patient’s point of view, the most important facts are simple.
Retinal tears are common enough that eye doctors see them regularly.
Retinal detachments are less common, but serious enough to be considered emergencies.
Treating tears early is one of the best ways to prevent detachments.
Who Is Most at Risk for Retinal Tears and Detachments?
Some people have a higher chance of developing these problems than others.
You are at higher risk if you have strong near-sightedness, a history of eye trauma, previous retinal tears or detachment in either eye, areas of lattice degeneration, or a family history of retinal detachment.
You are also at higher risk as you get older.
Age-related vitreous changes make tears and detachments more likely.
People with certain medical conditions, such as diabetes with advanced diabetic eye disease, can also develop retinal problems, including tractional detachments from scar tissue inside the eye.
If you fall into one of these groups, regular dilated eye examinations are especially important.
Your eye doctor can look for early changes, thin areas and small tears before they cause symptoms. Read more at American Academy of Ophthalmology patient information
Why Knowing the Risk Still Matters
Even though most people will never experience a retinal detachment, understanding the risk matters for everyone.
If you know that retinal tears and detachments can happen, you are more likely to recognise early warning signs.
If you understand that flashes, floaters and shadows are not normal, you are more likely to seek help in time.
Knowing that these problems are more common in certain groups can also guide you to regular eye care.
Preventive checks do not eliminate risk, but they can catch problems at a stage when treatment is easier and outcomes are better.
When Should You See a Doctor?
You should seek same-day eye care if you notice any of the following in one eye or both.
Sudden new flashes of light.
A sudden burst of new floaters.
A dark curtain, veil or shadow across your vision.
Sudden blurred or distorted central vision.
These symptoms do not mean you will definitely have a detachment, but they do mean your retina needs to be examined quickly.
Retinal tears and retinal detachment may not be common for every person, but they are common enough in eye clinics that doctors know how to recognise and treat them.
Quick action gives you the best chance to protect your sight.
Go To Retina Central